For years, “gut health” got filed under bloating and bathroom talk.
Then the science got louder.
Not in a woo-woo way, in a “this explains why your whole system feels off” way.
Because your gut is not just a tube that processes food. It’s a living ecosystem, an immune training ground, and a chemical factory that influences inflammation, metabolism, and even how resilient you feel mentally. ScienceDirect+1
Let’s break down what the latest research is actually pointing to, and why gut health is quietly becoming one of the highest leverage moves you can make for how you feel day to day.
1) Your gut is your body’s “border control”
Inside your intestines is a barrier that decides what stays in the gut, and what gets into the bloodstream.
When that barrier is strong: your body stays calm, your immune system doesn’t overreact, and digestion is smooth.
When it’s compromised: more inflammatory compounds can slip through, and you can end up with that vague “something’s off” feeling that shows up as low energy, skin flare-ups, mood swings, or chronic discomfort.
What’s wild is how fast this can shift.
A 2025 Immunity study found that within 48 hours of a high-fat diet in mice, key protective immune cells in the gut (ILC3s) were impaired, reducing IL-22, a protein that helps maintain gut lining integrity. Translation: your gut defenses can weaken shockingly quickly when the inputs are rough. Cell+1
This is one reason people can feel noticeably different after a weekend of “whatever” eating, even if nothing dramatic changed on the scale.
2) Ultra-processed food isn’t just “empty calories”, it reshapes the ecosystem
Ultra-processed foods (UPFs) don’t just add sugar and oils.
They can change microbial diversity, alter gut metabolites, and stress the gut barrier. Reviews in recent years keep circling the same theme: UPFs are associated with dysbiosis (microbial imbalance) and increased gut permeability. PMC+1
And this is no longer just theoretical or niche.
A November 2025 cohort study in JAMA Oncology looked at 29,105 women under 50 who underwent endoscopy. The highest UPF intake was associated with 45% higher odds of early-onset conventional adenomas (precancerous polyps), compared to the lowest intake. JAMA Network+1
This doesn’t mean “UPFs cause cancer” in a simplistic way.
It’s a signal that the modern diet is not neutral. It’s biologically active, and your gut is where the first dominoes start to fall.
3) Your microbes produce compounds that affect inflammation, blood sugar, and more
Your gut bacteria break down fibers and plant compounds into metabolites, including short-chain fatty acids (SCFAs) like butyrate.
These metabolites are linked to anti-inflammatory signaling, gut barrier support, and broader metabolic effects. JCI+1
On the flip side, the gut can also generate metabolites associated with cardiovascular risk (one example often discussed is TMAO pathways), which is why researchers keep calling the microbiome a key player in heart health and systemic inflammation. PMC+1
The theme here is simple:
Your gut doesn’t just digest your food. It converts it into signals.
4) The gut-brain axis is real, but it’s not magic
The microbiome and the brain communicate through immune signaling, hormones, metabolites, and the vagus nerve.
And while the internet loves turning this into “fix your gut, cure your anxiety,” the responsible takeaway is more grounded:
There’s meaningful evidence of a relationship between gut patterns and well-being, and gut-targeted interventions show modest effects in some research, with big variability between studies. Nature+1
In other words: promising, not a silver bullet.
Still, for anyone who’s ever had a stressful week and then noticed their stomach immediately joins the chat, this is the science catching up to lived experience.
5) The most boring advice is still the most effective: fiber + fermented foods
If you want a gut-friendly blueprint that is both ancient and modern, it’s this:
1) Feed the good microbes
Fiber and prebiotic fibers are a major lever for shifting gut composition.
A 2025 randomized controlled trial in healthy adults found that four weeks of higher fiber intake shifted gut microbiota and improved bowel-related quality of life (and even looked at secondary outcomes like sleep and skin). PubMed+1
2) Add fermented foods
A Stanford diet intervention found a fermented-food diet increased microbiome diversity and decreased inflammatory markers (compared to a high-fiber group in that specific study design). Stanford Medicine+1
If your gut health has felt “stuck,” these are the two biggest, most repeatable dials.
So where does Mojo fit into this?
Here’s the honest problem we kept seeing in our community:
People know gut health matters… and then life happens.
You’re busy. You travel. You forget the fermented foods. Your fiber intake drops. Stress spikes. Sleep gets weird. Then digestion gets weird, then everything feels harder than it should.
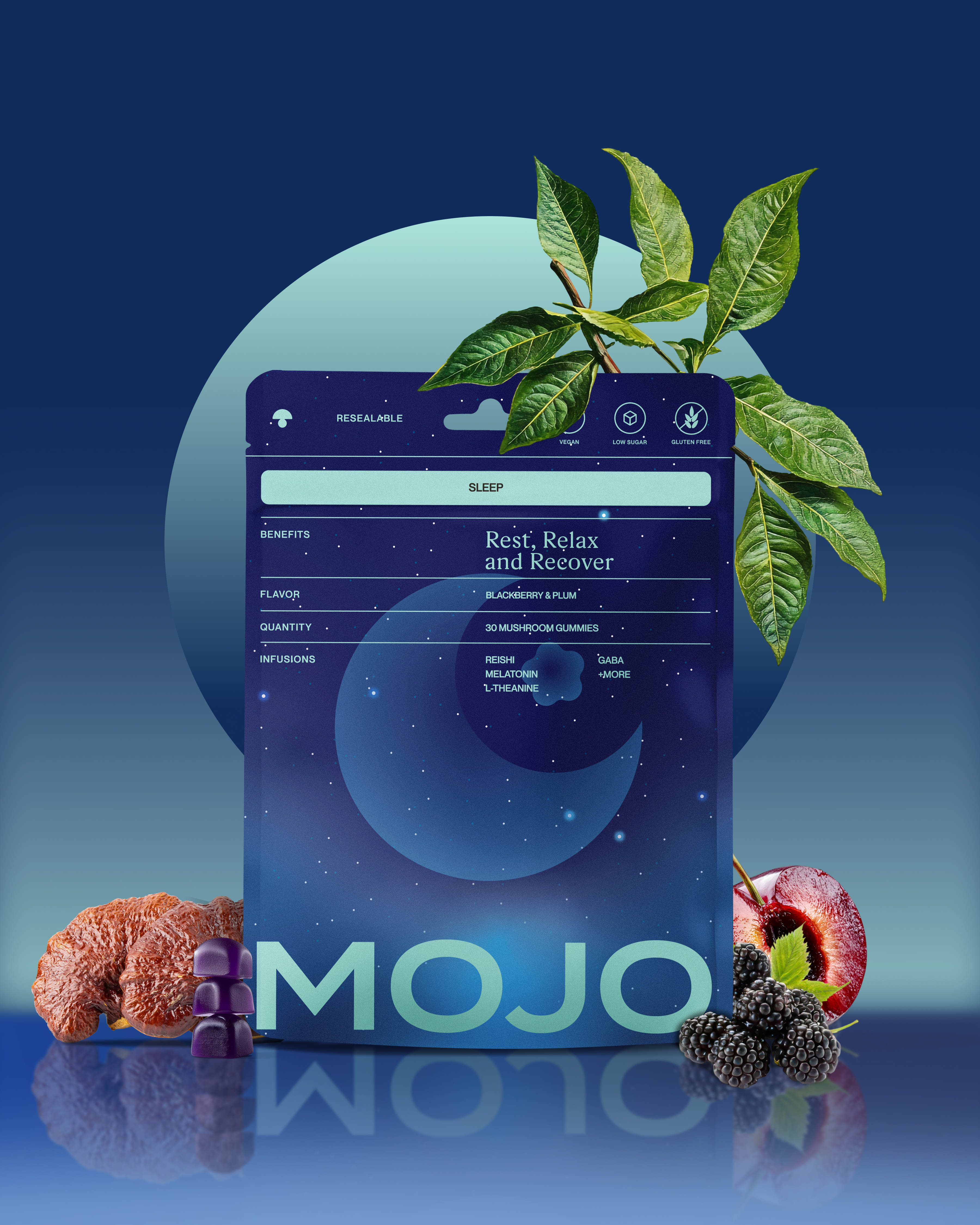
That’s why we built our new Mojo Gut Health gummy as a daily “baseline” support. Not as a magic fix, and not as a substitute for real food.
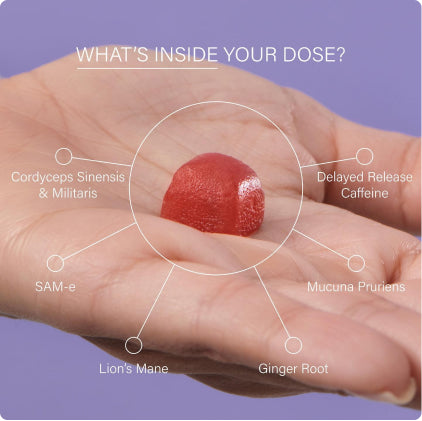
More like: a simple, consistent habit that stacks with the basics.
-
Prebiotic-style support (because feeding the microbiome matters)
-
Probiotics (with the reality that strains and consistency matter)
-
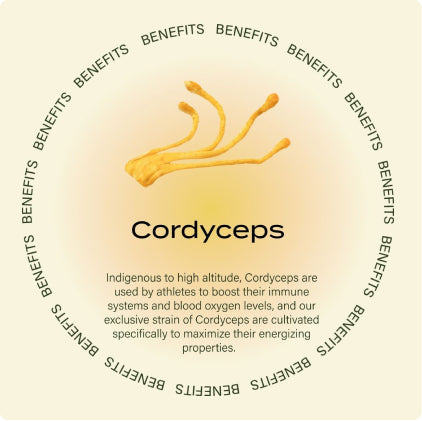
Botanicals, adaptogens, and functional mushrooms (because gut support is not just one ingredient, it’s a system)
And yes, we’re bringing it because you asked for it.
Massive demand from the community, and we’ve been obsessed with how gut health touches everything from digestion to inflammation to mood.
If you want first dibs, keep an eye on the launch updates. This one’s for the people who want to feel better from the inside out, without adding another complicated routine to their life.
Table of contents